Hey Diva dressing fans! When the items we love coincide with brands we work with, Diva dressing will use Paid Links in our articles. If you decide to click on these links and purchase the product, we get a small commission. Our Opinions Are Our Own, but we do add Paid Links as a way to offer these products at no added cost to our readers. Want to know more? Click Here to check out our Terms of Use anytime!
Postpartum depression (PPD) is a serious mental health condition that affects millions of new mothers every year. Unlike the “baby blues,” which usually pass after a few weeks, postpartum depression can last much longer and have significant emotional, psychological, and physical impacts. Alarming data from the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) suggest that the number of PPD cases is on the rise globally, including in the United States. This trend poses not only a challenge for affected mothers but also impacts their families, babies, and society as a whole.
Understanding why postpartum depression is becoming more common and how to address it is essential for supporting new mothers and promoting maternal mental health.
What is Postpartum Depression?
Postpartum depression is a type of depression that occurs after childbirth, typically within the first year but often within the first few months. It differs from the “baby blues,” which is a temporary emotional response many new mothers experience. While the baby blues involve mood swings, irritability, and tearfulness, they usually subside within a few weeks. In contrast, postpartum depression is more intense and can last much longer if left untreated.
The symptoms of PPD vary but often include:
- Persistent sadness or hopelessness
- Severe fatigue or lack of energy
- Difficulty bonding with the baby
- Feelings of guilt, worthlessness, or inadequacy as a mother
- Anxiety and panic attacks
- Changes in appetite or sleep patterns
- Thoughts of self-harm or harming the baby (in extreme cases)
While any new mother can experience PPD, those with a history of depression, lack of social support, stressful life events, or financial challenges may be at greater risk. It’s important to note that PPD can affect any woman, regardless of age, race, or socioeconomic status.
Why Are Cases Increasing?
Several factors contribute to the rising rates of postpartum depression, many of which are related to societal changes, economic pressures, and healthcare challenges.
One significant factor is the increasing societal and cultural pressures on new mothers to “have it all” and to excel in both their professional and personal lives. The unrealistic expectation to balance motherhood, career, and social responsibilities often leads to overwhelming stress, contributing to the development of mental health disorders. Social media can exacerbate this by promoting an idealized version of motherhood, which leaves many women feeling inadequate when their reality doesn’t match up.
The COVID-19 pandemic has also played a critical role in exacerbating mental health conditions, including postpartum depression. The isolation imposed by lockdowns and social distancing measures deprived many new mothers of vital support systems, such as family visits, community groups, and in-person healthcare appointments. Many women gave birth during periods of uncertainty, which increased their anxiety and made it more difficult to access mental health services.
Economic factors are another key driver. The cost of healthcare, lack of paid maternity leave, and pressure to return to work shortly after childbirth place additional stress on new mothers. Women from lower-income households may be more vulnerable to postpartum depression due to financial instability and reduced access to healthcare and mental health support.
Additionally, there is still a stigma surrounding maternal mental health, which prevents many women from seeking help. Women often feel pressure to “be strong” or worry that admitting to feelings of depression might make them seem like inadequate mothers. As a result, cases of PPD often go undiagnosed or untreated.
Impact on Mothers, Babies, and Families
Postpartum depression can have far-reaching effects, extending beyond the individual mother to her child and family. For the mother, untreated PPD can lead to chronic depression, anxiety disorders, and even suicidal thoughts. Many women experience an overwhelming sense of guilt, feeling as though they are failing their babies or their families, which only deepens their emotional turmoil.
For infants, the impact of a mother’s postpartum depression can be profound. Babies of mothers with untreated PPD may struggle to bond with their mothers, leading to developmental delays or emotional issues later in life. These infants are also more likely to have trouble sleeping, feeding, or thriving in the critical early months of life. Research has shown that children raised by mothers with untreated PPD are more likely to experience emotional and behavioral problems during childhood.
Postpartum depression also affects the family dynamic, placing strain on relationships between partners and other family members. Spouses or partners may feel helpless or overwhelmed, unsure of how to support the new mother. Without intervention, this can lead to tension, frustration, and a lack of communication within the household.
Treatment and Support
Fortunately, postpartum depression is treatable, and early intervention is key to ensuring positive outcomes for both the mother and her family. Treatment options include psychotherapy (such as cognitive-behavioral therapy), antidepressant medications, and support groups. Many women benefit from a combination of these treatments, along with increased support from their family and community.
Healthcare providers play a critical role in diagnosing postpartum depression. Routine screenings for PPD during prenatal and postpartum visits can help identify at-risk mothers before symptoms escalate. Encouraging open communication about mental health, reducing the stigma associated with depression, and providing accessible resources can help mothers seek the support they need.
Family and friends can also play a vital role by offering emotional support, assisting with childcare, and encouraging the mother to seek professional help when necessary.
Here are some products that can help
Mom Glass Plaque with Poem, Floral, Cursive Writing, Multi-Color, 4″ x 6.2 “x 3” $14.97

Mom/Spring Cookie Cutter Set – Multicolor $19.13

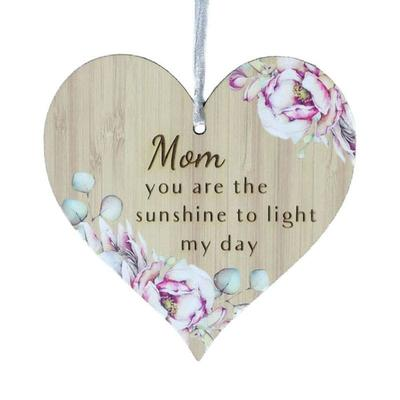
Floral Pattern Heart Shaped- Mom You Are The Sunshine To Light My Day Ornaments $23.98
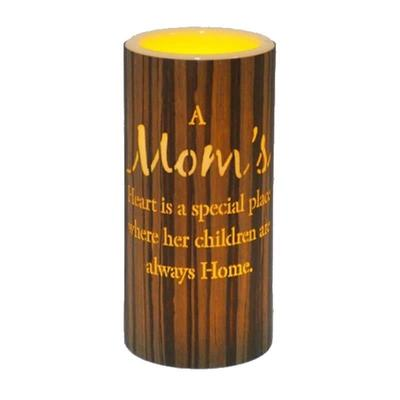
Led With Text- Mom Candle $25.99