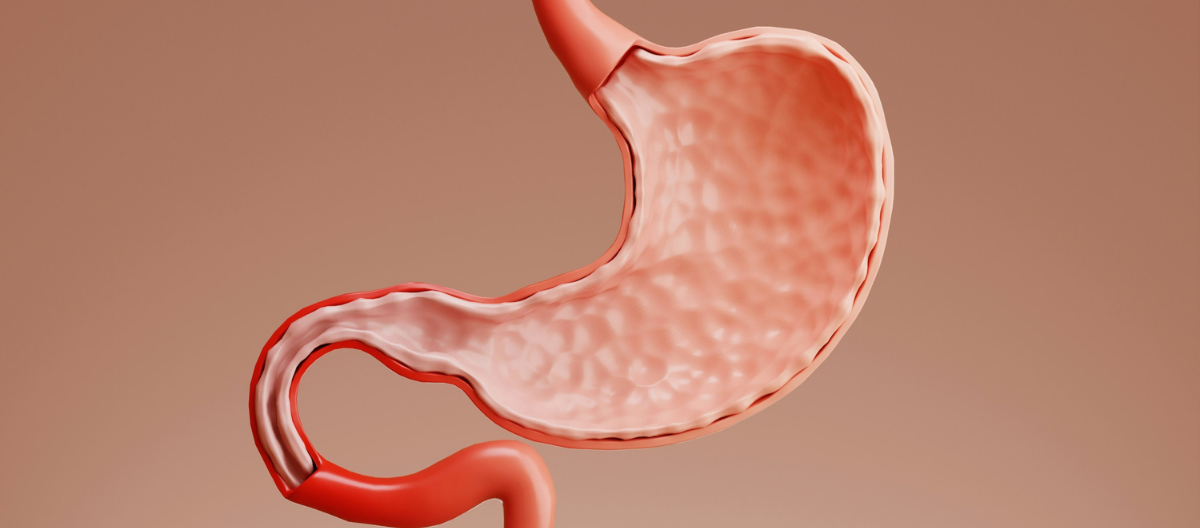
Digestive disorders encompass a wide range of conditions affecting the digestive tract, including the esophagus, stomach, intestines, and related organs. These disorders can significantly impact quality of life, causing discomfort and disrupting daily activities. Understanding common digestive disorders, their causes, symptoms, and treatment options is essential for managing and alleviating these conditions.
Common Digestive Disorders
Gastroesophageal Reflux Disease (GERD): GERD is a chronic condition where stomach acid frequently flows back into the esophagus, causing irritation. Symptoms include heartburn, regurgitation, chest pain, and difficulty swallowing. Lifestyle changes such as avoiding trigger foods, losing weight, and elevating the head during sleep can help manage GERD. Medications like antacids, H2 blockers, and proton pump inhibitors may be prescribed for more severe cases.
Irritable Bowel Syndrome (IBS): IBS is a functional gastrointestinal disorder characterized by abdominal pain, bloating, and changes in bowel habits, such as diarrhea, constipation, or both. Stress and dietary factors often exacerbate IBS symptoms. Management includes dietary modifications (e.g., low FODMAP diet), stress management techniques, and medications to address specific symptoms.
Inflammatory Bowel Disease (IBD): IBD encompasses two main conditions—Crohn’s disease and ulcerative colitis. Both involve chronic inflammation of the digestive tract, leading to symptoms like abdominal pain, diarrhea, weight loss, and fatigue. Treatment strategies include anti-inflammatory medications, immunosuppressants, and sometimes surgery. Dietary changes and stress management can also play a role in managing IBD.
Peptic Ulcers: Peptic ulcers are sores that develop on the lining of the stomach, small intestine, or esophagus due to the erosion caused by stomach acid. Common symptoms include burning stomach pain, nausea, and indigestion. Treatment typically involves medications to reduce stomach acid (e.g., proton pump inhibitors, H2 blockers) and antibiotics if the ulcers are caused by Helicobacter pylori infection.
Celiac Disease: Celiac disease is an autoimmune disorder where ingestion of gluten (a protein found in wheat, barley, and rye) triggers an immune response that damages the small intestine’s lining. Symptoms include diarrhea, abdominal pain, and malabsorption of nutrients. The primary treatment is a strict, lifelong gluten-free diet to manage symptoms and promote intestinal healing.
Diverticulitis: Diverticulitis occurs when small pouches (diverticula) in the colon become inflamed or infected. Symptoms include abdominal pain, fever, and changes in bowel habits. Treatment often involves antibiotics and a temporary liquid or low-fiber diet to allow the colon to heal. In severe cases, surgery may be necessary.
Gallstones: Gallstones are solid particles that form in the gallbladder and can obstruct the bile ducts, leading to pain and inflammation. Symptoms include sudden, intense pain in the upper right abdomen, nausea, and jaundice. Treatment options vary from dietary changes to medications that dissolve the stones, and in some cases, surgery to remove the gallbladder may be required.
Pancreatitis: Pancreatitis is inflammation of the pancreas, which can be acute or chronic. Symptoms include severe abdominal pain, nausea, vomiting, and fever. Treatment focuses on addressing the underlying cause (such as gallstones or alcohol use), providing supportive care, and managing pain. In chronic cases, lifestyle changes and medications to manage digestive enzyme deficiencies may be necessary.
Constipation: Constipation is characterized by infrequent, difficult, or painful bowel movements. Common causes include inadequate fiber intake, dehydration, and sedentary lifestyle. Treatment often involves dietary changes (e.g., increasing fiber and fluid intake), physical activity, and over-the-counter laxatives if needed.
Diarrhea: Diarrhea is characterized by frequent, loose, or watery stools. It can be caused by infections, food intolerances, or underlying conditions like IBS or IBD. Treatment includes staying hydrated, avoiding trigger foods, and using medications or probiotics to manage symptoms and restore gut health.
Diagnosis and Evaluation
Medical History: A thorough review of symptoms, dietary habits, and family history can provide insights into potential digestive disorders.
Physical Examination: The healthcare provider may perform a physical exam to assess abdominal tenderness, bloating, or other signs.
Diagnostic Tests: Various tests may be used to diagnose digestive disorders, including:
- Endoscopy: Involves inserting a flexible tube with a camera (endoscope) into the digestive tract to visualize and potentially biopsy affected areas.
- Imaging Studies: Techniques like ultrasound, CT scans, or MRI can help identify structural abnormalities or inflammation.
- Laboratory Tests: Blood tests, stool tests, and breath tests can provide information about infections, inflammation, and digestive function.
Treatment and Management
Medications: Various medications may be prescribed to manage symptoms, reduce inflammation, or address underlying causes. Common classes include antacids, proton pump inhibitors, antibiotics, anti-inflammatory drugs, and immunosuppressants.
Dietary Changes: Adjusting dietary habits can help manage symptoms and improve digestive health. This may involve eliminating trigger foods, increasing fiber intake, or following specific diets like the low FODMAP diet for IBS.
Lifestyle Modifications: Incorporating regular exercise, managing stress, and practicing good hydration can support overall digestive health and reduce symptoms.
Surgery: In some cases, surgical intervention may be necessary to treat conditions like severe IBD, gallstones, or peptic ulcers. Surgery may involve removing affected portions of the digestive tract or performing procedures to correct structural abnormalities.
Supportive Therapies: Complementary therapies such as probiotics, acupuncture, and cognitive-behavioral therapy may provide additional relief for certain digestive disorders.
Prevention and Self-Care
Healthy Diet: Consuming a balanced diet rich in fiber, fruits, vegetables, and whole grains supports digestive health and can prevent issues like constipation and diverticulitis.
Regular Exercise: Engaging in regular physical activity helps promote healthy digestion, reduce stress, and prevent weight-related digestive issues.
Stress Management: Managing stress through relaxation techniques, mindfulness, or counseling can help alleviate symptoms of stress-related digestive disorders like IBS.
Adequate Hydration: Drinking plenty of water supports overall digestive function and helps prevent constipation.
Routine Check-Ups: Regular visits to a healthcare provider can help monitor and manage any ongoing digestive issues and catch potential problems early.
When to Seek Medical Help
Consult a healthcare provider if you experience:
- Persistent or severe abdominal pain
- Unexplained weight loss
- Chronic diarrhea or constipation
- Blood in stool or vomit
- Difficulty swallowing or persistent nausea
- Unresponsive to over-the-counter treatments
Seeking medical advice ensures accurate diagnosis, appropriate treatment, and management of digestive disorders, leading to better health outcomes and improved quality of life.